How a name can make millions disappear
M.E. has more commonly been known as CFS or Chronic Fatigue Syndrome since the 1980s. However, this name has long been despised by the ME patient community due to its historical context and trivialising effect.
HISTORY
Myalgic Encephalomyelitis, or ME, was classified by the World Health Organisation Classification of Diseases as a Neurological disease in 1969. This name was coined after the London’s Royal Free Hospital outbreak.
"Myalgic" referred to the muscle symptoms; "encephalomyelitis" referred to the various neurological symptoms.
Despite the WHO classification (now ICD-10, G 93.3) there were many who did not believe that ME was a true neurological disease. In the 1970s, two psychiatrists in the UK, McEvedy & Beard - without interviewing any of the patients - reviewed 15 ME outbreaks and wrote a paper for the British Medical Journal (BMJ), where they concluded that the outbreaks were due to “mass hysteria”.
Despite the work and advocacy of Dr Melvin Ramsay - who believed in the biological basis of ME, the shadow cast by the BMJ article was too great (Shepherd, 2015).
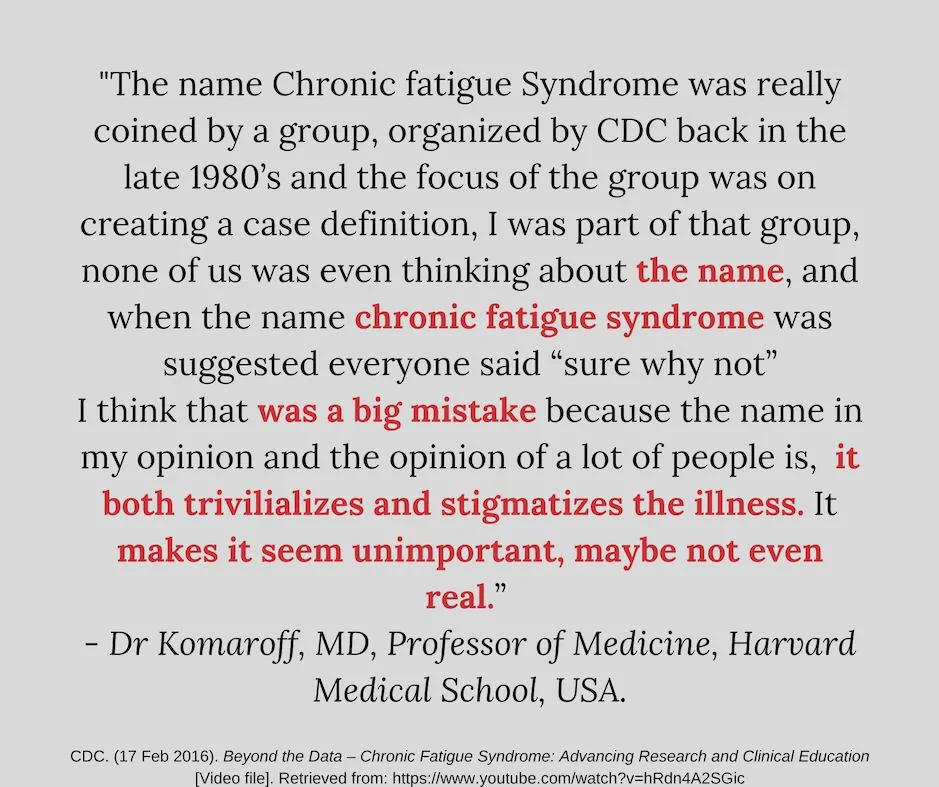
In this context, a new and thoughtless name ‘Chronic Fatigue Syndrome’ or ‘CFS’ came into being (by the CDC in the US and by UK psychiatrists 1991), along with new and more unspecific diagnostic criteria (Fukuda 1994 and Oxford 1991) that made CFS a wastebasket for all manner of fatiguing illnesses. All this would have dire consequences for ME patients for the next 30+ years. CFS “trivialised a serious medical condition – the equivalent of trivialising dementia by calling it a chronic forgetfulness syndrome – and shifted the focus from a “disease” to a single symptom, "chronic fatigue".” (IOM, 2015), (Shepherd, 2015)
A powerful body of psychiatrists with a historical professional bias toward misdiagnosing neurological conditions as mental health disorders (e.g. Multiple Sclerosis, MS, as paralytic hysteria; Epilepsy as hysteria), “convinced the medical profession that CFS was basically a mental health problem whereby people became trapped in a vicious circle of abnormal illness beliefs and behaviours, inactivity and deconditioning”. In other words, a somatoform disorder or psychosomatic disease, which in short, suggested that there was no real "biological disease" present….it was just in their heads. This “simplistic and seriously flawed model” (Shepherd, 2015) of ME causation gave birth to the PACE trial (Read our ‘CBT, GET & PACE Trial 2011’ summary under ‘Management’ here) and has also led to significant biases in the medical and scientific communities that have seriously harmed people with ME and irreversibly delayed research progress - by decades - that would have otherwise far sooner allowed for a better understanding of ME, discovery of a biomarker, and a potential cure.
Notes:
i) 85-90% of pwME want the name CFS to be changed (IOM, 2015) and are reclaiming the name ‘ME’. The most common complaints from people with ME are that this name is stigmatizing for them and causes others to question the legitimacy of their illness. CFS leads health professionals to minimise and dismiss their patient's concerns, as well as think that their patients are malingering (pretending to be ill for gain). It also trivialises the illness so that people with ME are continually faced with the ‘I’m tired too’ response when they tell people they have CFS.
ii) There have been some slow changes, e.g. an extensive review of CFS literature and research in the US (by the CDC in 2017) which led to a recommendation that the name be changed to ME/CFS, but unfortunately, the damage done by the stigma attached to this disease will linger for a long while yet.
iii) The name ‘SEID’ or Systemic Exertion Intolerance Disease that was put forward as a potential name change back in 2015 by the Institute of Medicine has been deemed to be just as unhelpful as CFS and has not been widely accepted.
References
IOM (Institute of Medicine). (2015). Beyond myalgic encephalomyelitis/chronic fatigue syndrome: Redefining an illness. Washington, DC: The National Academies Press.
Shepherd, C. (2015, Dec 07). It’s time for doctors to apologize to their ME patients. The Telegraph.